5 Key Takeaways from the Quality Payment Program by Year’s End
The Merit-based Incentive Payment System (MIPS) comes under the direct obligation of the Medicare Access and CHIP Reauthorization Act (MACRA), the law that regulates the incentive program across the US. It is the practical start of the value-based care model.
Eligible clinicians (ECs) have a responsibility to report MIPS 2019; they include physicians, osteopathic practitioners, chiropractors, physician assistants, nurse practitioners, and registered dietitians or nutritionists among others. To summarize, providers are to fulfill the low-volume threshold to qualify for MIPS 2019 reporting. Moving on to MIPS 2020, your next goal has its own set of requirements.
MIPS in healthcare gauges a clinician’s performance in terms of care delivery and reduced expenses. In this article, we come to an understanding of five key elements in relation to this program. In fact, the following data correlates with the preliminary data findings released by CMS on July 11, 2019.
Two Branches for Positive Payment Adjustments
The Quality Payment Program (QPP) 2019 branches out into MIPS and Advanced Alternative Payment Models (APMs). Whichever path you choose, it results in incentives for eligible clinicians, clinician groups, and virtual groups.
Furthermore, MIPS & MACRA go side by side; it is the popular track with stats and reports going in its favor. MIPS incentives for 2019 are less as compared to incentives in MIPS 2020. On the whole, the program is evolving, but once it does, it will be the birth of an improved healthcare system.
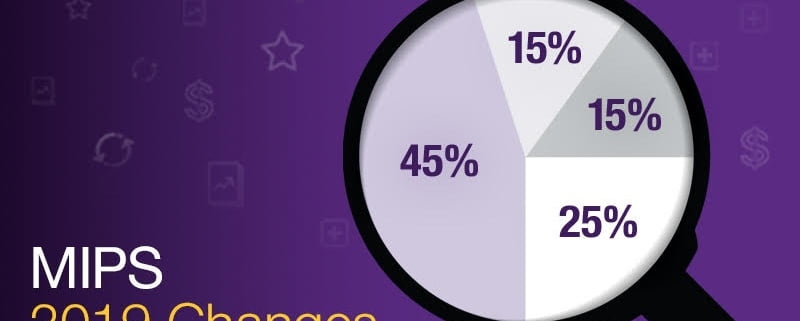
It divides into four performance categories as Quality, Promoting Interoperability (PI), Improvement Activities (IA), and Cost. Each category has certain measures that have to be reported through a MIPS Qualified Registry, CMS Web Interface, EHR, or Qualified Clinical Data Registry (QCDR). Not to forget, there is another catch to it in the form of collection types, which are the actual measures according to their submission systems.
Participation Level Increases Each Year
Since the start of the program in 2017, the participation level has gradually increased. It showed an increase from 95% in 2017 to 98% in 2018. Moreover, MIPS 2019 is only going to give us more eligible clinicians participating in it. The whole program suggests progression with higher participation levels across the country.
Small Practices Clinician Participation Status
According to the Centers for Medicare & Medicaid Services (CMS), 90 percent of clinicians from small practices engaged in MIPS 2018 which was 81 percent in 2017. So, that’s a 9% increase.
The primary flexibilities introduced in the Physician Fee Schedule (PFS) rule for the 2018 performance year included an increase in Medicare patient count and Medicare Part B allowed charges.
What did it mean?
It meant fewer clinicians from small practices were eligible to report MIPS in 2018. On the contrary, they decided to report it anyway. It goes to show that the system adjusted itself with practitioners’ convenience.
It was mentioned in a blog post by Seema Verma, Administrator CMS on July 11, 2019.
Advanced APMs Are Not Far Behind
Alternative Payment Model’s (APM) participation level isn’t far behind that of MIPS. CMS reports twice an increase of participants in 2018 as compared to 2017. There were 99,076 total participants in 2017, while the number doubled to 183,306 in 2018. We attribute this jump to new participation opportunities in 2018, especially through ACOs in the Medicare Shared Savings Program.
Even if we are to condemn MIPS in general, I can’t see any downside to opportunities and hope that clinicians continue to grab MIPS incentives year after year.
Spectacular Results So Far
The program collects incentives for the participating clinicians year after year, but the payout occurs one year after the performance year. For example, the payout for MIPS 2017 happened in 2019 in which 93 percent of the participants received positive payment adjustments.
Similarly, MIPS 2018 participants will receive a payout in 2020 which is almost here. CMS reports that 97 percent of the clinicians will be the owner of positive payment adjustments in 2020 based on their performances in 2018.
P3 Healthcare Solutions, Ontario, CA keeps an eye on what goes around as the MIPS performance period 2019 enters the final stages.
















Leave a Reply
Want to join the discussion?Feel free to contribute!