MIPS 2018 Updates For Clinicians And Healthcare Providers
The MIPS 2018 will help the healthcare providers realign themselves to ensure compliance, enabling them to keep taking advantage of the incentive payments.
CMS gave an update on 2nd November 2017, sharing MIPS 2018 updates applicable to the QPP (Quality Payment Program).
A Background to the MIPS 2018 Updates
We all know that there is a shift in the US healthcare industry towards quality healthcare. These new updates reflect the refinement of the policies for QPP while taking into consideration the US healthcare industry’s transformation concerning infrastructure, technology, clinical practices, and physician support practices.
MIPS 2018 Updates & QPP Strategic Payment Program Objectives
CMS aims to accomplish 7 strategic QPP objectives with the introduction of MIPS 2018 Updates.
- To assist in the overall improvement of beneficiary outcomes. It also means engaging patients by deploying relevant MIPS and Advanced APM policies.
- The improvement in the clinician experience through the introduction of a transparent and flexible program. This approach will help provide clinicians with easy-to-use program tools.
- Increase adoption and availability of the robust Advanced APMs.
- Maximize participation and understanding of the program by deploying customized communication that focuses on support, education, and outreach. The underlying theme is to ensure the program fulfills the needs of diverse types of practices, patients, physicians, and small healthcare providers.
- To promote the increased sharing of data and information relating to the program’s performance. Thus, the underlying concept is ensuring timely yet accurate availability of actionable feedback to clinicians and other relevant stakeholders.
- Help deliver IT systems with improved capabilities relating to reporting, data submission, and an overall improvement in its front and backend, delivering greater efficiency and value.
- Lastly, one of the core strategic QQP objectives is to improve program implementation and foster ongoing development that keeps the requirements of the US healthcare industry in context. Furthermore, it also helps small and rural healthcare providers successfully take part in the program.
What are the MIPS 2018 Updates?
Let’s look at the highlights of MIPS 2018 updates.
- Performance Period
- The performance period is changed from 90 days to a 12-month calendar year.
- The cost will be applicable based on the 12-month calendar year.
- A minimum of 90 days period will be under review for Advancing Care Information.
- A minimum of 90 days period will be under consideration for evaluating Improvement Activities.
Performance Threshold or Payment Adjustment
- Minimum Performance Threshold will consider 15 instead of 3 points.
Road to accomplishing 15 points for performance threshold
Here is how you can attempt to accomplish the 15 points. You can fulfill any one of these criteria to reach the goal of 15 points.
- To submit 6 Quality Measures that meet data completeness criteria.
- To meet the base score for Advancing Care Information. To accomplish it, you will have to submit 5 base measures and also submit a medium-weighted Improvement Activity.
- To meet the base score for Advancing Care Information. Also, submit 1 Quality Measure which meets data completeness requirements.
- Lastly, you can also reach the 15-points performance threshold goal by reporting all Improvement Activities.
- For achieving exceptional performance, the providers must reach the threshold of 70 points.
- The law requires the payment adjustment for the 2020 payment year to range between -5% to +5X% (where +5% means = 5% X scaling factor). The scaling factor is achieved to ensure the accomplishment of budget neutrality.
- Under the revised MIPS 2018 updates, the adjustment factor applies to items and services under Medicare Part B (It includes Part B drugs too).
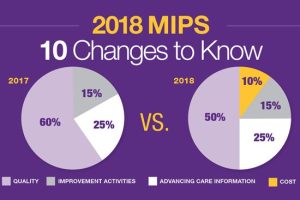
Quality
- The 2018 Quality Measures Specifications will become applicable.
- The weight of the final score is 50% instead of 60%.
- For Data Completeness, CMS wants providers and clinicians to meet a minimum threshold of 60% instead of 50%. Therefore, measures not meeting this data completeness criterion will only get 1 instead of 3 points. However, small healthcare practices will still get 3 points.
- The scoring has a 3-point floor for measures against the benchmark. There are 3 points for measures that either do not have a benchmark or they do not meet the case minimum requirement. Measures that fail to meet data completeness requirements will only get 1 point and not 3 points, except small practices getting 3 points. There is no change introduced for the bonuses. One of the MIPS 2018 updates is that CMS proposes the introduction of a cap of 6 points for a particular set of 6 topped out measures.
- The improvement scoring will be given by measuring the rate of improvement. The increase in improvement will mean more points, particularly for the providers that have a lower performance during the transition year. The improvement will be measured in the Quality Performance Category Level, with ten percentage points available for Quality Performance Category.
- One of the MIPS 2018 updates is about the topped out measures scored with a maximum of 7-points and not the standard 10-points.
6 topped out measures for 2018
- #21. To either select the Prophylactic Antibiotic-First or Second Generation Cephalosporin.
- #23. Venous Thromboembolism Prophylaxis, when they are indicated in all the patients.
- #52. COPD (Chronic Obstructive Pulmonary Disease), Inhaled Bronchodilator Therapy.
- #224. The overutilization of the Imaging Studies in Melanoma.
- #262. Confirmation via image, of successful excision of Image Localized Breast Lesion.
- #359. To optimize patient exposure by utilizing Standardized Nomenclature for CT (Computerized Tomography), imaging description.
Improvement Activities
- The providers must be aware of the specifications of the 2018 Improvement Activities.
- The weight to the final score will be 15%.
- There isn’t any change in the number of activities that MIPS eligible clinicians need to report for reaching 40 points. CMS wants to propose more activities to select from and also wants changes to existing activities for Inventory. The clinicians practicing in rural areas and small practices would only be needed to report no more than 1 high-weighted or 2 medium-weighted activities for reaching the highest score.
- For the TIN to get credit for group participation, only one MIPS eligible clinician would have to perform the Improvement Activity.
Advancing Care Information
- The providers and clinicians must be aware of the specifications for the 2018 Advancing Care Information Measures.
- The weight to the final score is 25%.
- To allow the MIPS eligible clinicians to use either the 2014 or 2015 Edition of CEHRT in 2018. And also to grant them a bonus if they only use the 2015 Edition of CEHRT.
- To add exclusions for the Health Exchange Measures and E-Prescribing.
- To add more Improvement Activities which would show the use of CEHRT to the list eligible for a bonus of Advancing Scare Information.
- One can earn 10% in performance scores if they report about any of the criteria to clinical data registry or single public health agency.
- An additional 5% is allocated for submitting to one additional clinical data registry or public health agency (not reported underperformance score).
- To add decertification exception for those eligible clinicians who’s EHR has been decertified, retro effectively for 2017 performance periods.
- The deadline for exception application submission for the year 2017 and for future years, is set on December 31st for measuring the whole year’s performance.
- Small practices which have 15 or fewer clinicians, the addition of a new category for hardship exceptions to re-weight the category of Advancing Care Information to 0. To reallocate the 25% of the category weight of Advancing Care Information to the category of Quality Performance.
- CMS will reweight the category of Advancing Care Information to 0 and reallocate its 25% performance category weight to the category of Quality Performance for these reasons.
- Automatic Re-weighting
- Certified registered nurse anesthetists, clinical nurse specialists, physician assistants, and nurse practitioners.
- The non-patient facing clinicians include pathologists and radiologists.
- The hospital-based MIPS eligible clinicians.
- The ASC (Ambulatory Surgical Center) – based MIPS eligible clinicians and the certified registered nurse anesthetists.
- To reweight through an approved application.
- There are significant hardship exceptions, and CMS will not be applying a five years limit for these exceptions.
- A new hardship exception to the clinicians practicing in small practices has 15 or fewer clinicians.
- There is a new decertification exception added for the eligible clinicians whose EHR has been decertified and becomes effective retroactively for the performance period of 2017.
Cost
- There will be a weight of 10% added to the final score.
- CMS will include the total per capita cost measures and MSPB (Medicare Spending per Beneficiary) for calculating the Cost performance category score for the MIPS performance period of 2018. These two measures will be carried over from the Value Modifier Program. These two programs are also currently used for providing feedback for the MIPS transition year.
- CMS will be calculating the cost measure performance. The clinicians do not need to take any action.
- The new changes offer Virtual Groups with participation options for Year 2, providing clinicians with another way to participate in MIPS. The Virtual Groups can contain Solo Practitioners and Groups containing 10 or fewer eligible clinicians. They are eligible to participate in MIPS, coming together virtually with at least one such other Solo Practitioner or Group for participating in MIPS. In general, clinicians being part of a Virtual Group would have to report as a Virtual Group for four different performance categories. They will also need to meet the same performance category requirements and measures as that the non-virtual MIPS groups.
- Virtual Groups need to conduct their elections at the beginning of the performance period. It cannot be changed once the performance period starts.
- Groups and Solo Practitioners wanting to participate in a Virtual Group have to go through the election process.
- The period given for election is from October 11thto December 31st, 2017, for them to be considered for the 2018 MIPS performance period.
- To increase the low volume threshold by excluding individual clinicians or groups eligible for MIPS having < $90,000 in Part B allowed charges. It is also applicable to those individual clinicians or groups with < 200 Part B beneficiaries falling within the low volume threshold determination period occurring during a performance period or a prior period.
- CMS is not changing the way it defines non-patient facing clinicians. Individuals <100 patient-facing encounters, and for groups, it stands at > 75% NPI’s billing under the group’s TIN falling within a performance period and labeled as non-patient facing.
- Under the Complex Patients Bonus, there is an adjustment applied to up to 5 bonus points by adding the average HCC (Hierarchical Conditions Category) risk score to the final score. The score addition would be anywhere from 1 to 5 points given to the clinicians depending on the patient’s medical complexities.
- The Small Practice Bonus will adjust the final score of an eligible clinician or group working in a small practice as defined in the regulation, applicable to 15 or fewer clinicians. It would add 5 points to the final score provided an eligible clinician or group submits the data for at least one performance category within the applicable performance period.
- There are payment adjustments by CMS for Extreme and Uncontrollable Circumstances, approximately given to 572,000 eligible clinicians. They would have to participate in MIPS for the 2018 MIPS performance period. Under the newly proposed rule, the payment adjustment for the 2020 payment year may range from =5% to +5X%. (X is the adjustment factor that allows MIPS program for staying budget neutral.)
- If the CEHRT for an MIPS clinician is unavailable due to uncontrollable circumstances like a natural disaster, public health emergency, or hurricane, etc. the clinician can submit a hardship exception application for getting reconsidered for reweighing of the Advancing Care Information performance category. The application is due with a cut-off date of December 31st, 2017.
- There is a final rule with a comment period extending this reweighting policy for the performance categories of Improvement Activities, Cost, and Quality which starts with the 2018 MIPS performance period. The deadline for this hardship exception application is December 31st, 2018.
As far as 2018’s submissions are concerned, the deadline was April 2, 2019. Moving on, if you were eligible back then, you are eligible in 2019 as well.
MIPS consulting services job is to satisfy your end of the deal with the authorities for compliance and data completeness. That is what we do for our clients!
Moreover, those of you who weren’t eligible then may be eligible now. Give us a call or simply fill up the form on the homepage to notify us. P3 Healthcare Solutions connects clinicians to high scores which means rewards and a better reputation.
QPP 2019 is prevailing and it is important to submit measures against Quality, Meaningful Use (MU) or Promoting Interoperability (PI), Improvement Activities, and Cost performance categories. With the promise of less reporting burden by CMS, we can expect the program to become clinician-friendly as time goes by.
What is next?
What changes to expect in MACRA-MIPS 2019?
For questions out of this knowledge base, or on instructions on how to get started call a MIPS specialist today at 1-844-557-3227 (1-844-55-P3CARE) or email at info@www.p3care.com.
















What are the key updates and changes introduced in the MIPS (Merit-Based Incentive Payment System) for clinicians and healthcare providers in 2018?